By Karen Bonfanti Davison, RN, BSN, OCN
Chemotherapy is a mainstay in the treatment of cancer and may be used alone or in combination with other treatment approaches, such as radiation and surgery, to combat the disease.
However, while chemotherapy can be highly effective, it often comes with side effects of varying types and degrees.
At Penn Medicine Princeton Cancer Center, certified oncology nurses specially trained in the administration of chemotherapy offer patients various methods to help reduce common side effects, including fatigue, nausea and hair loss.
If your doctor has recommended chemotherapy as part of your cancer treatment, you likely have concerns about what to expect. Here are answers to some of the most asked questions about chemotherapy and its side effects.
What is chemotherapy and how does it work?
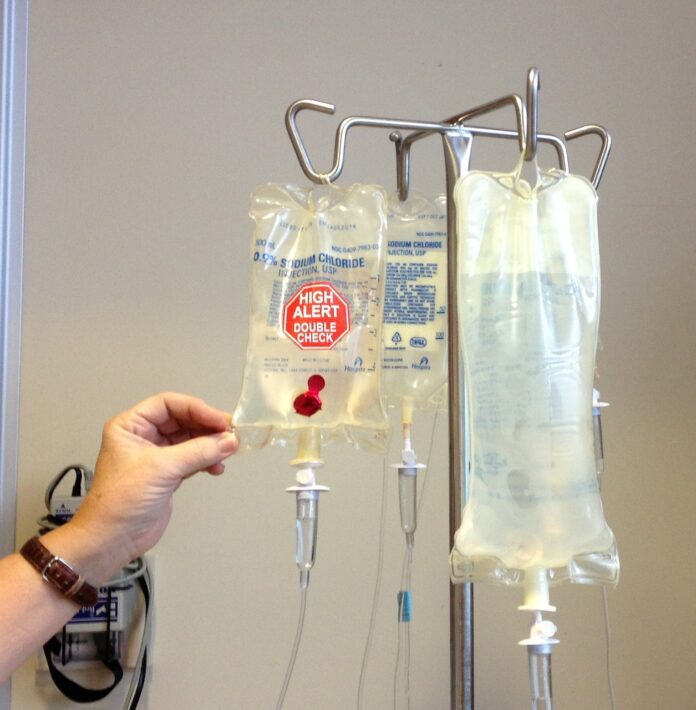
In short, chemotherapy is the use of powerful drugs to destroy cancer cells and prevent their growth and spread within the body. These drugs can be administered orally, through injections or intravenously.
The drugs work by targeting rapidly dividing cells, which is characteristic of cancer cells, and disrupting their ability to grow and multiply. There are many types of chemotherapy drugs, and each interferes with cell growth at a different step. Certain chemotherapy drugs are given only for certain diseases.
How is chemotherapy used as part of a treatment plan?
A major advantage of chemotherapy is its ability to treat widespread or metastatic cancer, whereas surgery and radiation are limited to treating cancer that are confined to specific areas.
Depending on your type of cancer and its stage of development, chemotherapy may be used for different purposes as part of your overall treatment plan.
- Primary treatment. In some cases, chemotherapy may be the primary treatment for cancer, especially if the cancer has spread extensively or when surgery or radiation isn’t feasible.
- Adjuvant therapy. Following surgery or radiation therapy, chemotherapy may be used to kill any remaining cancer cells and reduce the risk of cancer recurrence.
- Neoadjuvant therapy. Sometimes, chemotherapy is administered before surgery or radiation therapy to shrink tumors, making them easier to remove or treat with other methods.
- Palliative care. In advanced stages of cancer, chemotherapy can help alleviate symptoms, control the growth of tumors and improve quality of life by slowing disease progression.
Will chemotherapy make me tired and nauseous?
Fatigue, nausea and vomiting can all be side effects of chemotherapy.
In cases of fatigue, the medicine itself may cause tiredness. Moreover, in addition to destroying cancer cells, chemotherapy may destroy healthy red blood cells. If too many healthy cells are destroyed, it could lead to anemia, which causes tiredness.
Though it may seem counterintuitive, many people are able to combat fatigue by staying active. Low impact activities, such as taking a walk outside, practicing yoga, or working out in the garden, can all help boost energy levels.
Staying hydrated by drinking enough water and avoiding alcoholic and caffeinated beverages can also help combat fatigue.
Additionally, chemotherapy drugs can irritate the stomach lining leading to nausea and vomiting. In many cases, anti-nausea medications can be administered prior to chemotherapy to help manage symptoms. Patients may receive anti-nausea medicine to take at home after treatment and use as needed.
Some patients also benefit from aromatherapy with peppermint to help relieve symptoms.
What will chemotherapy do to my immune system?
Just as chemotherapy may destroy healthy red blood cells, it may also destroy healthy white blood cells, which help fight infection. If your white blood cells dip too low, you are more susceptible to colds, flus and other illnesses and resulting complications.
You can protect yourself by washing your hands regularly and avoiding crowds, especially seven to 10 days after your treatment when the drugs and your body are really working their hardest to fight the disease. You might also consider wearing a mask during that time.
What about neuropathy?
Some chemotherapy medications, such as taxanes commonly used for breast cancer treatment, may cause neuropathy in your hands and feet. To help protect the nerve cells and prevent neuropathy, patients may benefit by using cooling gloves, mittens and socks. A form of cryotherapy, a treatment that uses very cold or near freezing temperatures, cooling gloves, mittens and socks — equipped with gel packs — typically require freezing for a set amount of time before wearing. Cryotherapy works by constricting the blood vessels to reduce chemotherapy drug distribution and side effects.
Will I lose my hair?
Many chemotherapy drugs can cause hair loss, although not all do. Hair loss is often temporary, and hair typically grows back after treatment ends.
To help prevent or reduce hair loss in patients, Penn Medicine Princeton Cancer Center offers scalp hypothermia, commonly referred to as a cool or cooling cap.
Like cooling gloves, mittens and socks to prevent neuropathy, it is believed that scalp hypothermia constricts blood vessels in the scalp and therefore reduces the amount of chemotherapy that reaches the hair follicles. Moreover, the cold slows the activity of the hair follicle, making it less of a target for chemotherapy.
The cooling cap system at Princeton Cancer Center comprises two caps, an inner cap that is equipped to circulate cool liquid delivered by a computer-controlled compact refrigeration unit and an outer neoprene cap that prevents cold from escaping.
Prior to treatment, patients are fitted for the cap to ensure it is the right size and fits snugly on their head. On the day of treatment, patients wear the cap for 30 minutes prior to their infusion (pre-cool), during their infusion (cooling) and for 90 minutes after their infusion (post cool).
Patients using the cooling cap system need to follow certain practices in caring for their hair, including not dying their hair and not using heat-styling tools.
According to the American Cancer Society, recent studies of women getting chemotherapy for early-stage breast cancer have found that at least half of the women using computer-controlled cooling cap systems lost less than half of their hair.
As part of Penn Medicine, Princeton Cancer Center provides patients full access to the specialized clinical services, rehabilitative care, and support they need during treatment and recovery from cancer. The experts at Princeton Cancer Center work closely with teams at the Abramson Cancer Center, a world leader in cancer research, patient care and education, to provide patients access to advanced diagnosis and treatment.
For more information about Penn Medicine Princeton Cancer Center, visit princetonhcs.org/cancer. To find an oncologist affiliated with Penn Medicine Princeton Health, call 1 (888) 742-7496 or visit princetonhcs.org/directory.
Karen Bonfanti Davison, RN, BSN, OCN, is an oncology nurse navigator at Penn Medicine Princeton Cancer Center.